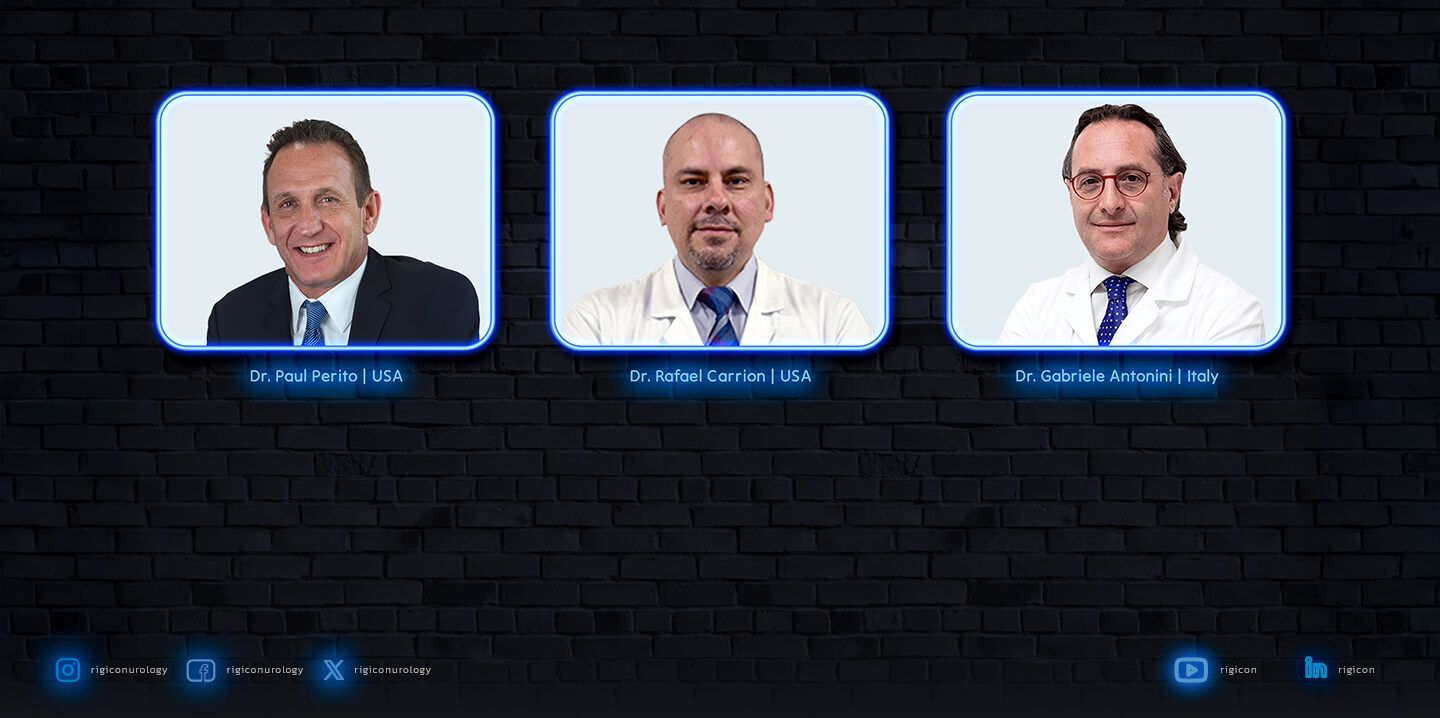
Welcome back to the Rigicon Academy Blog, where we spotlight international thought leadership and innovation in prosthetic urology. In this edition, we bring you a recap of the Prosthetic Urology 2022 Kickoff Webinar, recorded live on January 5, 2022. Esteemed experts Dr. Paul Perito, Dr. Rafael Carrion, and Dr. Gabriele Antonini shared their nuanced perspectives on surgical techniques, patient outcomes, and the evolving standards of care in penile prosthesis implantation.
From Miami to Rome, these world-renowned surgeons explored the common ground and differences in surgical approaches while agreeing on one core principle: surgical excellence, regardless of the technique, delivers optimal results when guided by experience and protocol.
Surgical Philosophy: “A Well-Done Implant Is a Well-Done Implant”
Dr. Perito initiated the session with a message of unity: while techniques may differ, a meticulously performed penile implant procedure consistently yields high patient satisfaction. He emphasized outcome-driven care over procedural dogma, advocating for collaboration in refining standards across approaches.
“There’s a common ground we can all stand on—regardless of the incision. A well-done implant is a well-done implant.”
The Infrapubic Approach: Precision, Speed, and Patient Comfort
Dr. Perito presented compelling data from his high-volume practice, noting that over 80% of patients resume sexual activity within three weeks post-op. He attributed this accelerated recovery to minimal dissection, avoidance of Foley catheters, and targeted use of drains.
Key Benefits:
- Earlier sexual rehabilitation: 82% at 4 weeks; currently trending toward 3 weeks.
- Reduced discomfort: Foley catheters often omitted entirely or removed before the patient wakes.
- Efficient exposure: Achieved within 2–3 minutes using pediatric specula and refined retractors.
- Safer reservoir placement: Closer proximity with less risk using a 70mm nasal speculum.
- Minimal dorsal nerve risk: Thanks to hydrodilatation and precise instrument handling.
- Pump positioning education: Teaching patients to pull the pump down reduces migration.
“I want penile implants to be as accepted as breast implants—routine, accessible, and stigma-free.”
The Penoscrotal Perspective: Visibility and Versatility in Complex Cases
Dr. Carrion highlighted the value of the penoscrotal approach, especially for complex revision surgeries, fibrosis cases, or teaching environments. While this method may involve more vascular exposure, it allows for adjunct procedures and precise pump fixation.
Key Highlights:
- Superior exposure in teaching cases and fibrosis.
- Ease of adjunct procedures like web takedown or vasectomy.
- Pump fixation using anchoring sutures for long-term positioning.
- Adaptability: Allows for longer incisions when anatomical variance demands it.
“It’s not a race. It’s about quality and letting your outcomes speak for themselves.”
European Innovation: Dr. Antonini’s Minimally Invasive Evolution
After training with Dr. Perito in Miami, Dr. Antonini transitioned from penoscrotal to infrapubic techniques, applying a minimally invasive philosophy. With patients often returning to function faster, his adaptations aim to further improve hemostasis, recovery, and cosmetic outcomes.
Technique Enhancements:
- Two additional sutures on the corpora to prevent hematoma.
- Drain placement for 3–5 days to minimize scrotal swelling and allow early device activation.
- Aesthetic incisions under 2 cm for improved cosmetic recovery.
- Customized “scratch technique” for Peyronie’s disease, correcting curvature while preserving function.
“We aim for less pain, fewer complications, and better recovery. Patients cycle the device within 2 weeks.”
The Future: Dedicated Centers & Standardized Protocols
All three surgeons emphasized the importance of:
- High-volume specialized centers for prosthetic urology.
- Structured patient education on expectations, postoperative care, and complications like hypermobility.
- Standardization of technique to improve outcomes globally.
As the field continues to evolve, collaboration between experienced surgeons, tailored training programs, and shared data remain essential to pushing the boundaries of what penile prosthetics can achieve—for both patients and practitioners.
Final Thoughts
The Prosthetic Urology 2022 Kickoff Webinar demonstrated how collaboration across surgical philosophies can advance the field and improve patient outcomes worldwide.
With thought leaders like Dr. Perito, Dr. Carrion, and Dr. Antonini paving the way, the field of prosthetic urology is in skilled and visionary hands.
🩺 Stay tuned for more educational content from Rigicon Academy.
All trademarks, registered marks (® and ™), and product names mentioned in this article are the property of their respective owners. The use of such marks does not imply any affiliation with or endorsement by them. This content is for informational purposes only and should not replace professional medical advice. Always consult with a qualified healthcare provider before making any decisions regarding your health.