Welcome to the Rigicon Academy Blog, where we delve into the latest developments in prosthetic urology and surgical technique. In today’s article, we explore a fascinating comparison between two surgical approaches to inflatable penile prosthesis (IPP) implantation—penoscrotal and subcoronal—as performed at the University Hospital Schleswig-Holstein (UKSH), Campus Kiel.
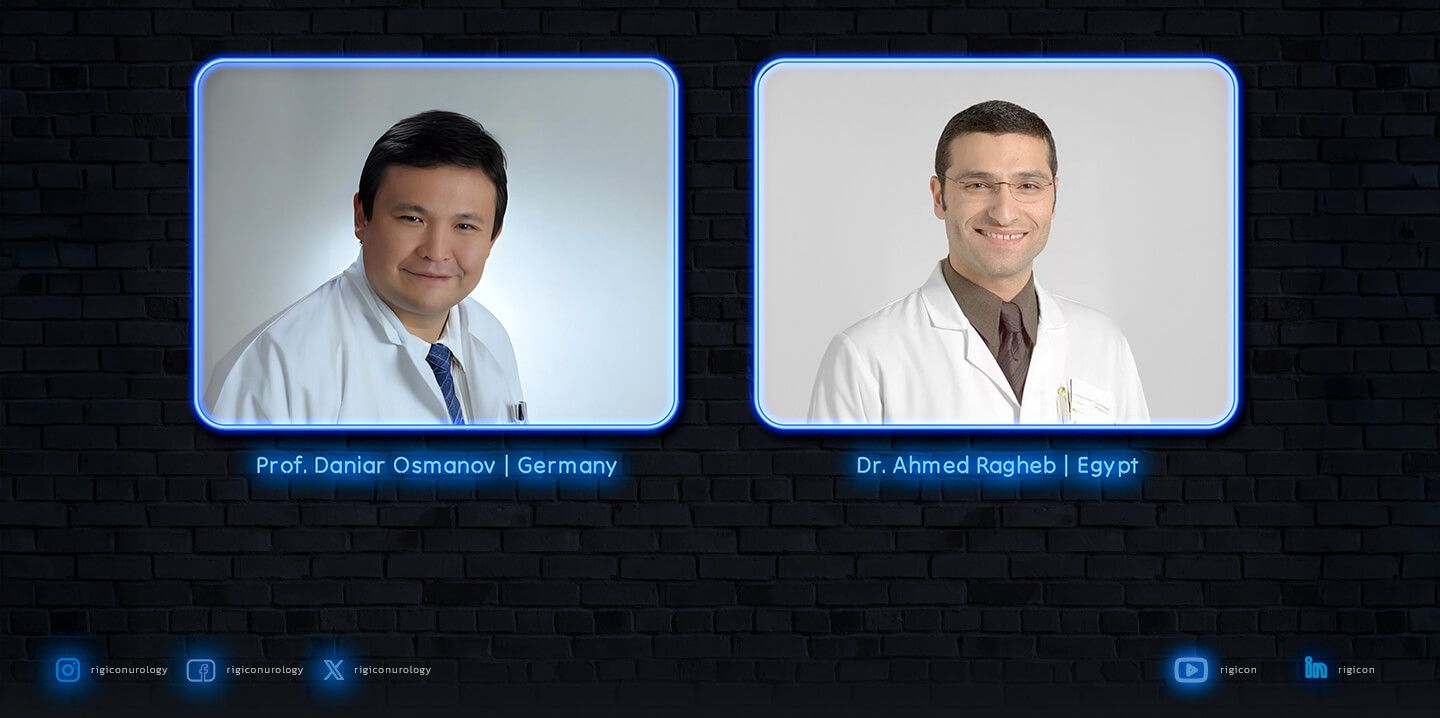
This topic was also discussed at the Rigicon Symposium during ESSM 2021, where Dr. Ahmed Ragheb and Dr. Daniar Osmonov presented their experiences and insights into advanced penile prosthetic techniques, highlighting the advantages of flexible approaches in complex surgical cases.
Case Study 1: Penoscrotal Approach
71-year-old male with post-radical prostatectomy erectile dysfunction, non-smoker.
A traditional transverse penoscrotal incision was used. Through careful dissection of Buck’s fascia and the tunica albuginea, the corpora cavernosa were accessed. This approach allowed optimal placement of implant tubing to reduce the risk of nerve injury.
Precise measurements were taken using a Furlow introducer—10 cm distal, 12 cm proximal on both sides. A size 18 cm Infla10® Pulse™ prosthesis was selected. Rear Tip Extenders (RTEs) of 3 cm and 1 cm were used to reach a total length of 22 cm.
“All components were dipped in a rifampin (60 mg) and gentamicin (120 mg) antimicrobial solution. The device’s hydrophilic coating and fourth-layer reinforced cylinders offer both durability and a natural feel.”
The reservoir was placed ectopically, and tubing was tunneled posteriorly with Babcock forceps. A closed suction drain was used postoperatively, and a “mummy wrap” compression bandage was applied.
Outcome: The penis was left partially inflated overnight, ensuring hemostasis. Recovery was uneventful.
Case Study 2: Subcoronal Approach
58-year-old male with 21-year diabetes, Caverject-induced corporal fibrosis, 10 pack-year smoking history.
This approach began with a circumferential subcoronal incision and full degloving of the penis. Exposure allowed access to the tunica albuginea for effective corporotomy.
This technique is particularly useful in patients undergoing simultaneous procedures, such as those for Peyronie’s disease, or in cases where general anesthesia is contraindicated.
The same Infla10® Pulse™ prosthesis with identical RTE sizing was used. A standard retropubic reservoir placement was performed, and the pump was placed in a subdartos pouch created through blunt dissection.
Outcome: Reduced scrotal trauma and potential for earlier device cycling due to minimized swelling.
Why Surgical Technique Matters
“With hands-on experience and proper training, urologists can provide life-changing outcomes through penile prosthesis surgery.”
Final Thoughts
Prosthetic urology is both a technical and emotional discipline. From cancer survivors to men with diabetes-related ED, restoring sexual function means restoring confidence and dignity.
With leading-edge devices like the Infla10® Pulse™ and a commitment to precision surgery, the future of erectile dysfunction treatment is stronger than ever.
This message was echoed at the ESSM 2021 Rigicon Symposium, where Dr. Ragheb and Dr. Osmonov underscored the value of global collaboration and advanced prosthetic innovation in improving patient outcomes.
🩺 Stay tuned for more surgical insights, real-life cases, and innovations from the Rigicon Academy.
All trademarks, registered marks (® and ™), and product names mentioned in this article are the property of their respective owners. The use of such marks does not imply any affiliation with or endorsement by them. This content is for informational purposes only and should not replace professional medical advice. Always consult with a qualified healthcare provider before making any decisions regarding your health.